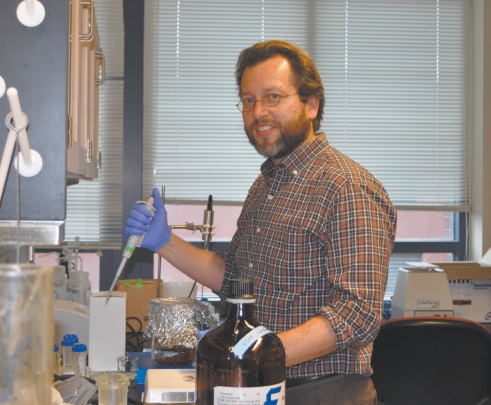
Professor Researches Cure for Alzheimer’s
For the past three years UWT professor, Dr. John Finke, has been creating antibodies to find a cure for Alzheimer’s disease. Finke and other biochemists have been utilizing genetic manipulation using mice to discover what may cure the disease.
Finke is from Washington State, but completed his undergraduate in Biochemistry at Claremont-McKenna College and graduate degree in Chemistry at the University of California, San Diego (UCSD). After graduating UCSD, he conducted further work as a Post-Doctoral Researcher in the UCSD physics department.
Finke was a professor at Oakland University in Michigan from 2005- 2012. In 2012, he came to UWT to study the immune system and its response to unfolded proteins linked to Alzheimer’s disease, otherwise known as senile dementia.
“UWT is kind of special,” Finke says. “It’s unlike many other university systems.”
The ability to work at a university in the midst of rapid growth that lacks structural barriers universities usually have across departments, separating them, is something Finke described as “unique.”
“You get to talk to people you usually don’t,” Finke said.
He has spent three years at UWT tweaking the chemical “jewelry” that decorates antibodies to discover how the immune system responds to misfolded proteins (which usually have modified or toxic functionality) when these surface groups are changed. Finke’s research is funded by the National Institute of Health. With help from students and research collaborators at the Veteran Affairs Hospital in Seattle, Finke has been investigating an unanswered question that has stalled progress towards a cure for Alzheimer’s disease.
“There is a layer of cells around the brain called the Blood Brain Barrier (BBB) and this is a very protective barrier, and very selective when letting things in,” Finke explains.
Although researchers have not found a sugar known as sialic acid plays a role in access through the BBB. In cases where the sialic acid is removed, such as viruses, the brain no longer allows the virus to enter. Finke describes the sialic acid as a possible “special password” that gets its molecular cargo through the BBB.
To test their theory, researchers have been using mice, who have a lot in common with humans, but do have different brains. Finke is exploring the ability of sialic acid, also used by the HIV virus, with a mouse model of Alzheimer’s Disease to help reach diseased cells in the brain. If the drug can get to the correct part of the brain, a cure might be found.
“When someone is infected with HIV they don’t want the molecule to enter their brain because it’s where the virus can hide, hang out, and evade by the immune system,” Finke said. “But perhaps the virus can teach us a thing or two about how we can design better drugs.”
He is hoping that if they can learn how the virus gets into the brain, Alzheimer’s drugs can use the same “trick” to get to where they are needed.
The primary animal used to test Alzheimer’s drugs before proceeding with the clinical trial with human patients is mice. “The mice are either genetically manipulated or bred to have Alzheimer’s symptoms in the brain, and early memory loss,” Finke said.
The mice don’t get Alzheimer’s, scientist create a similar disease with the hope that the cure that works on mice will also work on the human body.
After inducing the mouse with this protein, the creature goes through base memory testing exercise, which typically entails the mouse finding its way through a maze.
“It is unclear whether helping a mouse remember how to get through a maze, and treating that condition, is the same clinical approach that will help a senile human to remember who their family members are, or remember what their car keys are for,” Finke says. However, as with all experimental testing, it may just lead scientists to new breakthrough findings that will be of immense benefit to people struggling with Alzheimer’s in the future.